
When you first hear the words “abnormal spinal MRI,” it’s natural to feel a wave of anxiety. The spine is central to our mobility and well-being, and the thought of something being wrong with it can be alarming. However, an abnormal spinal MRI result doesn’t always spell disaster. In many cases, these findings are more benign than they appear. Here’s why an abnormal spinal MRI might not be as bad as you think.
1. Common Incidental Findings
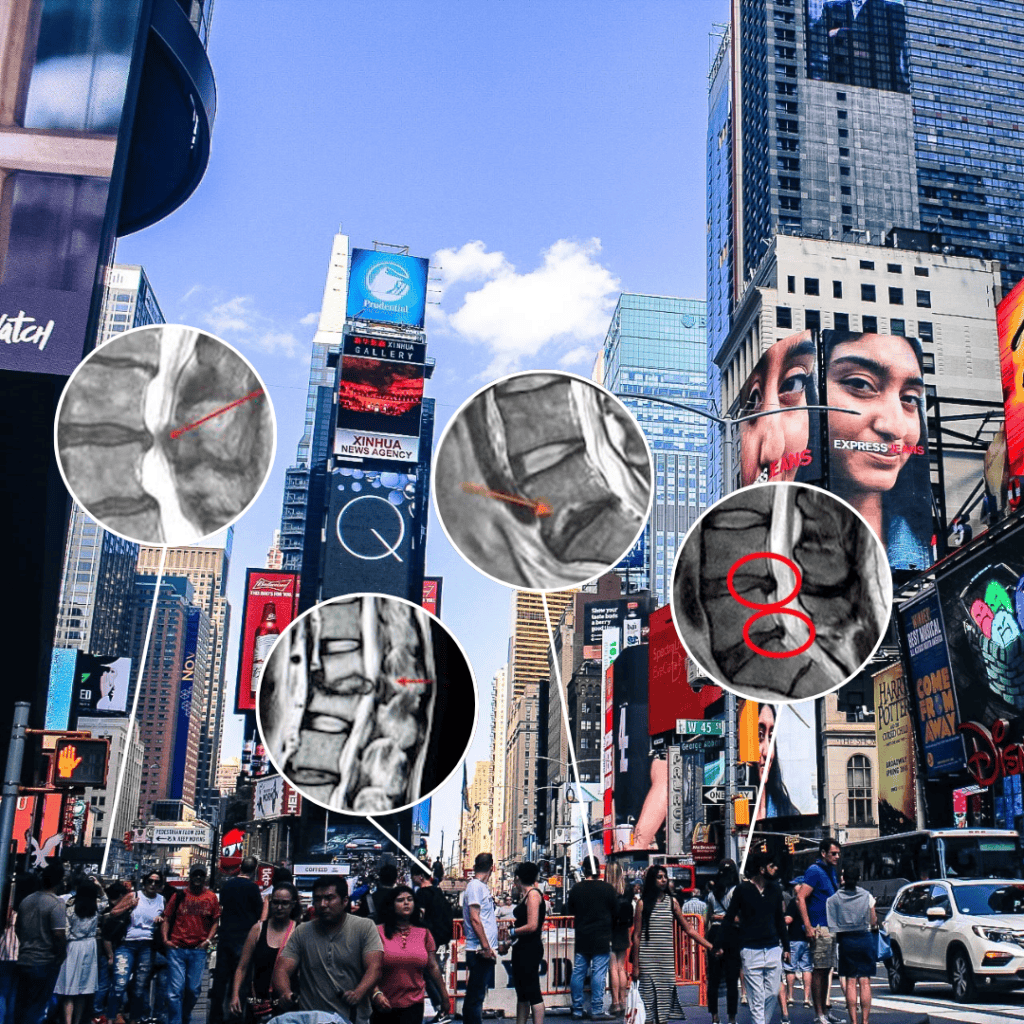
MRIs are incredibly sensitive and often detect minor changes that don’t cause any symptoms. These incidental findings are common and frequently do not require any treatment. They might sound concerning, but many of these findings are simply harmless quirks picked up by the highly detailed imaging.
2. Age-Related Changes Are Normal
As we age, our spines naturally undergo changes. Studies have found that many asymptomatic patients have numerous abnormalities on their MRIs, and the frequency of these findings correlates with age. For example, asymptomatic 50-year-olds may have conditions like degenerative disc disease, annular tears, herniated discs, stenosis, scoliosis, spondylolisthesis, kyphosis, facet cysts, Tarlov cysts, and adjacent level degeneration, among others. While these findings might sound concerning, these changes are often part of the normal aging process and do not necessarily indicate a serious condition.
3. Symptoms and Context Matter
Not all abnormalities cause symptoms. It’s crucial to correlate MRI findings with your symptoms, physical exam results, and other tests like EMG nerve conduction studies, X-rays, CT scans, or PET scans. This comprehensive approach helps determine the significance of MRI findings and ensures that any necessary treatment targets the actual cause of your symptoms.
4. Effective Treatments Exist
Even if an MRI shows an abnormality causing symptoms, many effective treatments are available. Physical therapy, medications, lifestyle changes, and targeted injections can often relieve pain and improve function. Surgery is usually a last resort and is considered only when conservative treatments have failed, and the condition significantly impacts quality of life.
5. Targeted Injections for Diagnosis
A good way to confirm the source of your pain is through targeted injections with an anesthetic such as lidocaine or bupivacaine, together with steroids. If the injection provides temporary pain relief, it helps identify the pain generator’s location. Make sure your surgeon performs these injections before considering spine surgery.
Conclusion
An abnormal spinal MRI doesn’t necessarily mean you have a severe problem. Many findings are incidental or age-related and may not cause symptoms. With proper medical guidance, comprehensive evaluation, and effective treatments, you can manage your spinal health and maintain a good quality of life. Always consult with a healthcare provider to understand your specific situation and the best steps forward. Remember, an MRI is just one piece of the puzzle, and your health journey is unique to you.
FAQ
What is the difference between lidocaine and bupivacaine? Lidocaine and bupivacaine are both local anesthetics, but they differ in onset and duration. Lidocaine has a rapid onset (1-5 minutes) and a short duration (1-2 hours). Bupivacaine has a slower onset (10-20 minutes) and a long duration (up to 8 hours).
What is annular tear? An annular tear is a tear in the outer layer (annulus fibrosus) of an intervertebral disc. The tear can cause pain, inflammation, and may lead to disc herniation. Symptoms often include localized back pain, pain radiating to the extremities, and in some cases, neurological symptoms if nerve roots are compressed.
What is degenerative disc disease (DDD)? Degenerative Disc Disease (DDD) is a condition characterized by the breakdown of intervertebral discs, which are the cushion-like structures located between the bones (vertebrae) of the spine. Despite its name, DDD is not a true disease but rather a condition that can result from the normal aging process, wear and tear, or injury. While it can lead to significant pain and disability for some individuals, a combination of conservative treatments, lifestyle modifications, and, in some cases, surgical interventions can effectively manage symptoms and improve quality of life.
What is a herniated disc? A herniated disc, also known as a slipped or ruptured disc, occurs when the soft inner gel-like center (nucleus pulposus) of an intervertebral disc protrudes through a tear or rupture in the tougher outer layer (annulus fibrosus). This condition can press on nearby nerves and cause pain, numbness, or weakness. Understanding its causes, symptoms, and treatment options can help manage the condition effectively. With appropriate care, most individuals can recover well and resume their normal activities.
What is stenosis? Stenosis refers to the abnormal narrowing of a bodily passage or orifice. In a medical context, it often pertains to the narrowing of spinal canal (spinal stenosis) or blood vessels (vascular stenosis), which can lead to a variety of symptoms depending on the location and severity of the narrowing. Understanding the types, causes, symptoms, diagnosis, and treatment options is crucial for effective management and improving patient outcomes.
What is scoliosis? Scoliosis is a medical condition characterized by an abnormal lateral curvature of the spine. The spine of an individual with scoliosis may look more like an “S” or “C” rather than a straight line when viewed from behind. This condition can occur at any age but is most commonly diagnosed in children and adolescents.
What is spondylolisthesis? Spondylolisthesis is a condition where one of the vertebrae in the spine slips out of place onto the vertebra below it. This slippage can cause pain, nerve compression, and other symptoms. The severity of spondylolisthesis can range from mild to severe. Many individuals find relief with conservative treatments and physical therapy. Surgery may be necessary for more severe cases, especially if there is significant nerve compression or instability. Early detection and appropriate management can improve quality of life and reduce the risk of complications.
What is kyphosis? Kyphosis is a spinal disorder characterized by an excessive outward curvature of the thoracic spine, resulting in a rounded or hunched back appearance. While some degree of kyphosis is normal, an exaggerated curvature (more than 50 degrees) is considered abnormal and can lead to various symptoms and complications.g to a hunched back appearance. Understanding its types, causes, symptoms, diagnosis, and treatment options is crucial for effective management. With appropriate care, many individuals can manage symptoms and maintain a good quality of life, while severe cases may benefit from surgical intervention to correct spinal deformity.
What are Tarlov cysts? Tarlov cysts, also known as perineural cysts, are fluid-filled sacs that form at the nerve root sheaths in the spinal canal, typically in the sacral region. These cysts contain cerebrospinal fluid and may result from congenital factors, trauma, or increased cerebrospinal fluid pressure. Many Tarlov cysts are asymptomatic and found incidentally during imaging studies. Symptomatic cysts can cause localized and radicular pain, numbness, tingling, weakness, and in severe cases, bladder, bowel, and sexual dysfunction.
Diagnosis involves medical history, physical examination, and imaging studies such as MRI or CT myelogram. Treatment options include conservative approaches like pain management and physical therapy, minimally invasive procedures like aspiration and fibrin glue injection, and surgical treatments such as cyst fenestration or microsurgical excision. The prognosis varies, with many individuals remaining asymptomatic, while others may require treatment to manage symptoms effectively. There are no known preventive measures for Tarlov cysts, but early detection and monitoring can help manage symptoms and prevent complications.
What are the latest minimally invasive treatments available? The spine is always changing but the most exciting thing is Endoscopic Spine Surgery. This surgery uses a small endoscope and instruments to remove herniated disc material or decompress nerves.
How can exercise and fitness decrease back pain and neck pain? Regular exercise and fitness can significantly reduce back and neck pain by strengthening core and back muscles, improving flexibility, enhancing posture, and increasing blood flow to spinal tissues. Maintaining a healthy weight through exercise reduces spinal stress and slows degenerative processes. Exercise also alleviates stress and improves pain perception. Specific exercises like yoga, Pilates, strength training, swimming, and Tai Chi are particularly beneficial. Always consult a healthcare provider before starting a new exercise regimen, especially if you have existing conditions or chronic pain.
What to do when you find out you have an abnormal MRI? Discuss the findings with your healthcare provider to understand the implications. MRI findings should be interpreted in the context of your clinical symptoms and physical examination. Additional tests may be necessary to clarify the diagnosis or rule out other conditions. Work with your doctor to develop a treatment plan that may include physical therapy, medications, or possibly surgical intervention.
Do young people have abnormal MRIs? Yes, young people can have abnormal MRIs. These abnormalities can be asymptomatic or associated with conditions like disc herniation, congenital spinal abnormalities, or early degenerative changes.
How often should an MRI be performed? The frequency of MRIs depends on the clinical situation such as acute conditions, chronic conditions and pre-surgical planning.
How recent should MRI be before surgery? An MRI should generally be recent, ideally within 3-6 months before surgery, to ensure that the images reflect the current status of the pathology and to assist in precise surgical planning.
Are MRIs dangerous? MRIs are generally safe as they use magnetic fields and radio waves instead of ionizing radiation, making them non-invasive and free of radiation risks. However, precautions are necessary for individuals with metal implants, claustrophobia, or specific conditions, and any concerns should be discussed with a healthcare provider. Do they have radiation? No.
Why do I need xrays and MRIs? X-rays and MRIs are essential diagnostic tools with different strengths. X-rays are excellent for visualizing bones and detecting fractures, while MRIs provide detailed images of soft tissues like muscles, ligaments, and nerves. Since no single imaging technique can show everything, using both X-rays and MRIs allows for a comprehensive evaluation of bone and soft tissue conditions. Is there a single imaging that shows everything? No.
Why do asymptomatic patients have so many abnormalities on MRI? Aging and natural wear and tear can lead to detectable abnormalities without causing symptoms.
Should I worry if my MRI shows abnormalities but I have no symptoms? Not necessarily. It’s important to consider physical symptoms and other diagnostic tests.
What are common spinal abnormalities found in asymptomatic patients? Degenerative disc disease, herniated discs, stenosis, and scoliosis are common findings.
How can targeted injections help in diagnosing pain? Targeted injections help diagnose pain by delivering anesthetics to specific areas to confirm the pain source. They differentiate between conditions, identify nerve involvement, and predict treatment response. This method avoids unnecessary treatments and allows for personalized pain management plans. Common injections include facet joint, epidural steroid, sacroiliac joint, and trigger point injections. These injections enhance diagnostic accuracy and guide effective treatment strategies.
What should I discuss with my surgeon before spine surgery? Before spine surgery, it is important to have a comprehensive discussion with your surgeon. First, understand your specific diagnosis and why surgery is recommended, including what alternative treatments have been considered or tried. Learn about the type of surgery, the technique to be used, and the goals of the procedure. Be aware of the potential benefits and risks, including possible complications. Ask about the surgeon’s expertise and success rates with the procedure.
Discuss any required preoperative tests, medication adjustments, and lifestyle changes you may need to make. Understand the type of anesthesia to be used and any associated risks, and consider meeting with the anesthesiologist to address any concerns. Know the expected recovery time, the rehabilitation plan, and pain management strategies. Learn about the success rates and long-term prognosis of the surgery.
Discuss the length of hospital stay, postoperative care arrangements, and the support you will need from family or friends during recovery. Finally, understand the overall cost of the surgery, including any associated expenses, and what costs will be covered by insurance. These discussions will help you make an informed decision and prepare adequately for the surgery and recovery process.
