What Is a Tarlov Cyst Excision?
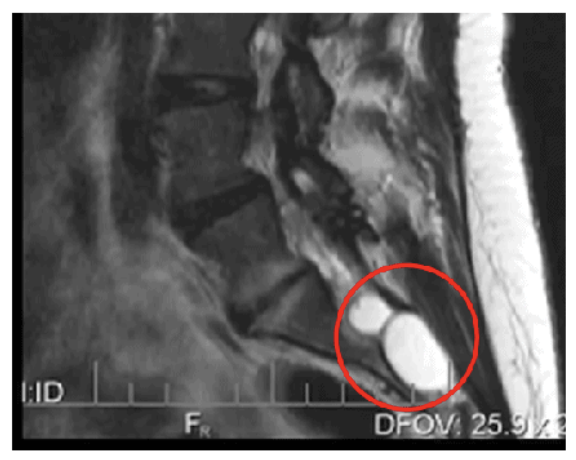
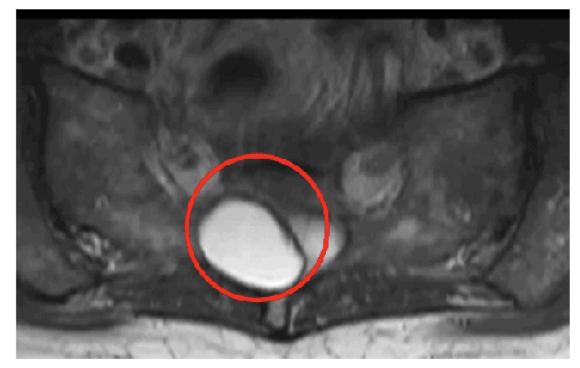
A Tarlov cyst excision is a minimally invasive spine procedure used to remove or reduce symptomatic Tarlov cysts, which are fluid-filled sacs that form around nerve roots, most commonly in the sacral region near the base of the spine. These cysts can compress nearby nerves and cause chronic pain, numbness, weakness, or dysfunction in the lower back, legs, bladder, or bowel.
During the procedure, the nerve root sleeve surrounding the cyst is carefully opened. Any small internal membranes or obstructions that prevent the normal flow of cerebrospinal fluid (CSF) are addressed. The sleeve is then imbricated, meaning the redundant tissue is folded and sutured to restore the normal shape and size. A dural patch is applied to reinforce the area and seal the CSF, helping to prevent fluid leakage or recurrence.
The surgery is performed using computer navigation and minimally invasive techniques, which allow for precise targeting with a smaller incision and faster recovery.
Why Is a Tarlov Cyst Excision Performed?
Tarlov cyst excision is performed to relieve symptoms caused by symptomatic Tarlov cysts, especially when conservative treatments have failed.
Typical symptoms of a symptomatic Tarlov cyst may include:
- Chronic lower back or sacral pain
- Radiating leg or buttock pain
- Numbness or tingling in the legs or feet
- Bowel, bladder, or sexual dysfunction
Before surgery is recommended, most patients undergo non-operative treatments such as:
- Physical therapy
- Pain medication
- Injections (nerve blocks or cyst aspiration)
If temporary relief is achieved with diagnostic injections but symptoms return, surgery may be considered as a definitive solution.
How Do You Prepare for a Tarlov Cyst Excision?
Preparation for surgery includes:
- Detailed imaging studies (MRI or CT myelogram) to evaluate the size, location, and characteristics of the cyst
- Review of medical history and confirmation that the cyst is the source of symptoms
- Discontinuation of certain medications, such as blood thinners, as advised
- Preoperative fasting if general anesthesia is required
- Arranging transportation and home support for the first few days after surgery
Your surgeon and care team will walk you through all pre-op instructions to ensure you are fully prepared and comfortable going into surgery.
What Can You Expect During a Tarlov Cyst Excision?
The procedure is performed under general anesthesia using real-time computer navigation to ensure precision. A small incision is made over the affected area, and the surgeon carefully accesses the cyst without damaging surrounding nerves or structures.
- The nerve root sleeve surrounding the cyst is opened.
- Any membranes interfering with CSF flow are removed or modified.
- The sleeve is imbricated (folded and sutured) to reshape and stabilize the area.
- A dural patch is placed to seal the area and prevent spinal fluid leakage.
The entire procedure is performed through a minimally invasive approach, which reduces trauma to nearby muscles and tissues.
Most patients are discharged the same day or after a brief overnight stay, depending on individual recovery.

What Is the Recovery Like After a Tarlov Cyst Excision?
Recovery varies depending on the size and location of the cyst, as well as the patient’s overall health, but most patients recover well with minimal downtime.
Immediately After Surgery:
- Patients are typically up and walking the same day or the following morning
- Pain is managed with oral medications
First 2 Weeks:
- You’ll be advised to avoid heavy lifting, bending, or twisting
- Rest and light walking are encouraged to promote healing
2 Weeks Post-Op:
- Physical therapy typically begins to support strength, mobility, and posture
4–6 Weeks Post-Op:
- Many patients are ready to return to work, especially if their job is sedentary
- For more physically demanding work, your surgeon will provide specific return-to-activity guidance
Your care team will monitor healing progress through follow-up appointments and imaging, if needed.
What Are the Potential Risks of a Tarlov Cyst Excision?
While Tarlov cyst excision is performed with precision and minimally invasive techniques, potential risks may include:
- Infection
- Bleeding
- Nerve irritation or injury
- Dural tear or cerebrospinal fluid leak
- Persistent or recurrent symptoms
- Scar tissue formation
These risks are uncommon, and your surgeon will take every precaution to reduce them and support a safe, successful outcome.
Are There Related Procedures to a Tarlov Cyst Excision?
Yes. Related procedures or alternatives may include:
- Tarlov cyst aspiration – temporarily draining the cyst (often diagnostic)
- Epidural steroid injections – to reduce inflammation
- Nerve root blocks – to identify the pain source and to help identify if the Tarlov cyst is causing symptoms
- Laminectomy or hemilaminectomy – if spinal decompression is needed in addition to cyst removal
Your surgeon will determine the most appropriate treatment approach based on your condition, imaging results, and response to prior therapies.
Key Takeaways About Tarlov Cyst Excision
- Tarlov cyst excision is a minimally invasive surgery that removes or repairs fluid-filled cysts pressing on spinal nerves.
- The procedure restores normal spinal fluid flow and relieves nerve compression.
- It is typically considered after non-surgical treatments have failed and when injections confirm symptom relief.
- Patients usually go home the same day, begin physical therapy in 2 weeks, and return to work in 4–6 weeks.
- Recovery is generally smooth, with less pain and quicker healing due to the minimally invasive approach.
Next Steps
If you’ve been diagnosed with a Tarlov cyst and are experiencing persistent symptoms despite non-surgical care, a Tarlov cyst excision may be the next step toward long-term relief. Schedule a consultation to discuss your options and determine whether this procedure is right for you.

