- Less muscle and tissue damage
- Decreased blood loss
- Reduced post-operative infection rate
- Less post-operative pain
- Shorter hospital stays
- Smaller scars
- Faster recovery time
- Quicker return to daily activities
- Dong Quai
- Echinacea
- Ephedra
- Fish Oils (Omega-3 Fatty Acids)
- Feverfew
- Garlic
- Gingko biloba
- Ginseng
- Goldenseal
- Kava
- Saw Palmetto
- St. John’s Wort
- Turmeric
- Vitamin E
- Valerian Root
- Aspirin
- Coumadin/Warfarin
- Effient/Prasugrel
- Pradaxa/Dabigatran
- Aggrenox/Dipyridamole
- Non-steroidal anti-inflammatory drugs (NSAIDS), such as Mobic/Meloxicam, Motrin/Ibuprofen/Advil, Naproxen/Naprosyn/Aleve, Ketorolac, Voltaren/Diclofenac, Celebrex (Note: Tramadol, and Tylenol/Acetaminophen are ok to take for pain control during this time)
- If you take a GLP-1 Agonist weekly, stop 1 week prior to surgery. These include: Dulagutide/Trulicity, Exenatide/Byetta or Bydureon, Liraglutide/Saxenda or Victoza, Lixisenatide/Adlyxin, Semaglutide/Ozempic/Wegovy/Rybelsus
- Plavix/Clopidogrel (Restart 72 hours after surgery)
- Eliquis/Apixaban (Restart 72 hours after surgery)
- Xarelto/Rivaroxaban (Restart 72 hours after surgery)
- Metformin
- If you take a GLP-1 Agonist daily, stop 1 day prior to surgery. These include: Dulagutide/Trulicity, Exenatide/Byetta or Bydureon, Liraglutide/Saxenda or Victoza, Lixisenatide/Adlyxin, Semaglutide/Ozempic/Wegovy/Rybelsus.
- ACE inhibitors (Lisinopril, Captopril, Enalapril, Sacubitril)
- Angiotensin II Receptor Blockers/ARBs (Losartan, Valsartan, Candesartan, Irbesartan)
- Please arrive at the hospital/facility at the time directed by the hospital/facility. This is usually 2 hours prior to your scheduled surgery.
- Remain NPO (no food and no water) as instructed.
- After checking in, you will be asked to complete any remaining admission or consent forms.
- You will then be escorted to the pre-operative holding area to be prepared for your surgery.
- You will be asked to change into a hospital gown.
- An IV line will be started, and an initial set of vital signs will be taken.
- The anesthesiologist will review your chart and answer any of your questions.
- Dr. Kim will meet with you to answer any last-minute questions and exchange/verify contact information with you and your family and/or friends.
- When the surgical team is ready, you will be taken to the operating room.
- The anesthesiologist will manage your vital signs and adjust your anesthetic as needed to ensure your comfort and safety throughout the entire time you are in the operating room.
- While you are sleeping, a small tube, called a Foley catheter, may be inserted into your bladder to drain urine during your surgery. This catheter is either removed while still in the operating room or may remain in place until you are up and out of bed if you are expected to stay in the hospital overnight.
- A neuromonitoring technician will apply electrodes to your arms and legs to monitor certain nerve signals intraoperatively.
- The surgical team will prepare you and place drapes to ensure a sterile environment.
- The total time required for surgery differs from patient to patient depending on the complexity of the procedure.
- You will be taken to a recovery area where you will remain for 1-2 hours.
- Dr. Kim will update your family and/or friends.
- You may feel groggy from the anesthesia.
- A nurse will monitor your vital signs and check your pain level. You should tell the nurse when it hurts, where it hurts and how much it hurts on a pain scale of 0-10.
- Your nurse will let you know when you are medically ready to leave and will review the discharge instructions with you.
- After your surgery, the nursing and surgery teams will closely monitor you.
- Generally, each day starts with a blood draw for routine monitoring.
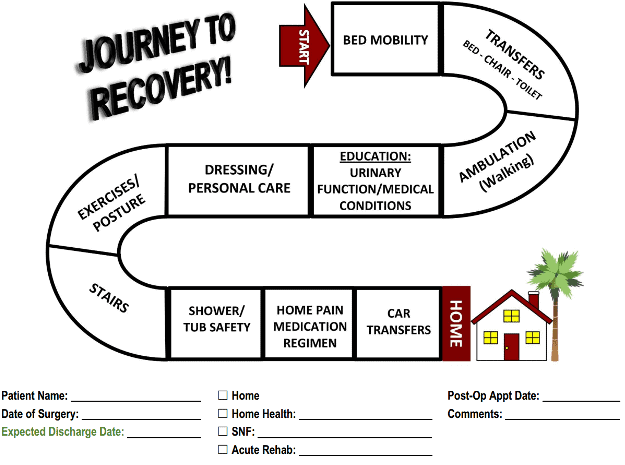
- You will be introduced to physical therapists, the two of you will work together to achieve important goals outlined in the “Journey to Recovery”, which was given to you at your pre-op appointment with Dr. Kim. These goals include regaining independence and mobility, developing a program for walking at home, and understanding proper body mechanics and spine precaution.
- A provider from Excel Spine will visit you.
- Most patients go home the afternoon of post-operative day #1.
Your stay at the hospital will depend on your individual condition, your tolerance to pain medication, and the extent of your surgery. Your individualized treatment “pathway” (also known as the “Journey to Recovery”) will outline your plan of care during your hospital stay. Most patients go straight home but some patients may need to recover in a skilled nursing facility (SNF) about 1-3 days after surgery.
After 3 days, remove the dressing and leave the incision open to air. Wash your hands before and after caring for your incision. Your incision has medical glue that dries purple and acts like a barrier to protect your incision. Let the glue flake off over the next up to 3 weeks; do not pick at the flakes. Wear a clean cotton T- shirt to keep the area dry. Do not apply creams, lotions, or ointments to the incision for the first 6 weeks. To avoid infection or scarring, do not scratch or scrub the incision. Please notify us of any discharge from the wound and email a photo of your wound and dressing if this occurs to Choll@excelspine.com. Please include the time of your last dressing change in the email so we can assess the quantity of discharge and recommend appropriate wound care. If you have been prescribed antibiotics, finish the entire prescription as directed.
- Change positions at least every 30-45 minutes.
- Stay active throughout the day, taking breaks when necessary.
- Take pain medication as directed and at least 30 minutes before planned activity or exercise.
- Apply a covered ice pack 2-3 times a day, for 15-20 minute intervals to help swelling or discomfort.
- Use relaxation techniques such as meditation, deep breathing, reading or listening to music.
- Perform simple stretches and gentle range of motion (ROM) exercises. See our YouTube Video on gentle back exercises that may be started before physical therapy: https://www.youtube.com/watch?v=FB5G_o0DRIQ
Some pain is to be expected as you recover. The amount and intensity of pain you may experience varies by the extent of the surgery and your tolerance to pain medications. Some patients find significant pain relief right after surgery and may only need to take Tylenol/Acetaminophen, while other patients experience a fair amount of residual pain and soreness that persists and slowly improves over time. These patients may need to take prescription pain medications for a few weeks after surgery. Be sure to take your medications as instructed and understand that some medications are to be taken only as needed. Common side effects of narcotic pain medications include constipation, nausea, drowsiness, and dizziness. It is important to wean off of all narcotic pain medications and transition to Tylenol/Acetaminophen as soon as possible to prevent narcotic dependence. However, do not take narcotic pain medication and Tylenol/Acetaminophen together because the narcotic medication may already have Tylenol/Acetaminophen in it. Do not take more than 3,000 mg of Tylenol/Acetaminophen in one day. Also, do not drink alcohol or drive while you are taking pain medication. Lastly, do not take aspirin-like products or non-steroidal anti-inflammatories (NSAIDS, outlined on pg. 4) for 3 months after surgery, unless Dr. Kim instructs you to do otherwise.
Try to sit in firm chairs with armrests and good back support. When going from a sitting position to a standing position, keep your back straight, scoot to the edge of the chair, place your feet firmly on the ground and use the armrests to help push yourself up. It is important to maintain good posture and to move slowly. Avoid soft sofas and chairs with wheels.
To regain your strength and speed your recovery, short frequent walks are encouraged. Walking strengthens your back and leg muscles, increases your endurance and relieves stress. Instead of taking one long walk, you should take several short walks throughout the day, and gradually increase the distance and frequency of your walks. You should also develop a regular walking routine and make it a habit for the rest of your life in order to maintain a healthy spine. Make sure to utilize proper body mechanics and use your pain/discomfort as a guide for most activities. If you experience increased pain for more than two hours after an activity, you’ve done too much too soon. When you feel pain, slow down and pay more attention to your posture and movements.
Avoid lifting more than 10 pounds for 4 weeks after surgery (a gallon of milk weighs about 9 pounds). When lifting, use proper body mechanics, try to only lift objects that can be easily lifted with one hand, and do not lift above your elbows. Do not participate in sports or activities that require frequent or strenuous bending, twisting, pushing or pulling (such as gardening, mowing the lawn, etc.) for about 2-3 months after surgery. When bending, try to use your knees rather than your waist, but you should try to bend and twist gently to avoid stiffness. Also, try to avoid climbing full flights of stairs until you are steady on your feet, and have enough strength and balance to do so safely. You should have help going up and down the stairs for the first few attempts. Start with one step at a time and use a railing. Listen to your body and be mindful of your limits.
You may walk around without restriction but be aware that your muscles are weaker after spine surgery and you may be more susceptible to falls. You should change positions throughout the day to help control pain, prevent blood clots and improve circulation. It is helpful to sit for a while, lie down for a while and take short walks periodically throughout the day. You should gradually increase your activity level and rest as needed. You should also perform gentle stretches and exercises on a consistent basis in order to increase flexibility, strengthen muscles and maintain an active lifestyle. Use common sense regarding activity. Do not push yourself to the point of fatigue or pain – moderation is the key.
You may sleep in any position you find comfortable. You should try sleeping on your back with a pillow under your knees, or on your side with a pillow between your knees and a pillow behind your body slightly tucked under your back and hips. To maintain good posture, avoid using more than two pillows under your head and try to keep your back straight.
A healthy, well-balanced diet will help strengthen your immune system, give you energy, increase your tolerance to activity, and help your incision heal. Be sure to increase fluid intake to six, 8 oz. glasses of water each day, and eat fresh fruits and vegetables high in fiber. This will help the common constipation caused by pain medication and inactivity. You should also take the bowel medications (Colace, Dulcolax) that were prescribed at your pre-operative visit to stay ahead of constipation or until you have your first bowel movement (then as needed).
It is always our goal that patients return home after spine surgery. Though, in some cases, patients may need help beyond what a family member or friend can provide. These patients may benefit from home health services including nursing care, physical therapy, and occupational therapy, which are brought to the patient’s home for a short period of time. During each visit, a nurse will check and record vital signs, examine the incision, assist with dressing changes, and teach the patient or the caregiver to do the same. The nurse will also go over medications, nutrition, fluid intake, and the regularity of bowel movements. In other cases, some patients may benefit from a short stay at a skilled nursing facility (SNF), especially patients who need help walking, caring for themselves, or do not have someone at home to assist them. Dr. Kim will determine if you may benefit from either of these services and they will be arranged for you prior to surgery.
If Dr. Kim orders you a brace, it will either be given to you at your pre-op appointment with Dr. Kim or a representative will deliver it to your home and fit it for you. A back brace is a temporary support and should only be used as needed for comfort. You should wear a clean loose cotton T-shirt under the brace to protect skin and absorb sweat. Do not wear the brace in bed. If Dr. Kim orders a walker, cane, toilet seat or commode, the hospital case manager or home health coordinator will order it for you at the time of discharge from the hospital. In many cases, patients do not need any equipment.
You may shower with the dressing. The dressing should be removed 3 days after your surgery and you may continue to shower with the incision uncovered. Let the soapy water run over the incision freely, but afterwards, make sure to dab it dry with a towel. It is important that you do not submerge the incision site in water, including bathtubs, pools and hot tubs, until the incision is completely closed (usually 6 weeks after surgery).
Your motivation and participation in physical therapy are essential elements of your recovery; you must play an active role in every step of your rehabilitation. You will receive a prescription for physical therapy at your first or second post-operative appointment with Dr. Kim. Outpatient physical therapy usually starts 4-6 weeks after surgery and continues for about 6 weeks. The goal is to establish and optimize an individualized home/gym exercise program that can be continued on a consistent basis even after your formal physical therapy is completed. This program will focus on improving functional mobility non-impact aerobic exercises, coordination and balance, proper body mechanics, and overall conditioning. As your physical therapy sessions draw to an end, the transition to your home/gym program should be seamless. Your dedication to physical therapy and exercise will set the pace for your recovery.
You may start a pool exercise program, go swimming, take baths and go in hot tubs around 6 weeks after your surgery. Please be sure to wait until your incision has completely healed before submerging it in water. If you are unsure, please email or text a picture of your incision to our office or Dr. Kim.
Around 3 months after surgery, you can begin chipping and putting. If chipping and putting are not painful, you may move to the driving range. Start with short-irons, move to mid-irons, and then to long-irons and clubs, as long as you are not experiencing pain at each level.
Driving will depend on the extent of your surgery and your recovery progress. Your pain must be managed so that you no longer need any narcotic pain medication, such as Percocet, Oxycodone, Vicodin, etc. These medications can affect your ability to drive. Generally, many patients can start driving after 4 weeks, but you should consult Dr. Kim. Try to limit initial driving to short, local distances.
This will depend on the extent of your surgery, your recovery process and the specific requirements of your job. If you have a relatively sedentary job and can comfortably sit, you may resume working around 6 weeks after surgery. If your job is physically demanding, and you are able to perform controlled exercises and lift weights, you may return to work around 3 months after surgery; however, more time may be needed. Dr. Kim recommends returning to work on a part-time basis with limited duties before returning to full-time work without any restrictions. If you need to take time off work, please contact your employer for FMLA forms. For more information about FMLA, visit: www.dol.gov/whd/fmla/.
Most patients wait to resume intercourse for about 4 weeks. You should situate yourself in a position that supports and takes pressure off the lumbar region. You can achieve this by lying flat on your back, placing a small pillow or hand towel under your low back, and placing a pillow under your knees to make them slightly bent. The bottom or missionary position is usually the safest and most comfortable; however, use your pain and discomfort as a guide.
You will follow-up with Dr. Kim or a Physician Assistant periodically throughout the next year to ensure that you are continuing to heal appropriately. Your first post-op appointment will be 1-2 weeks after surgery. During this appointment, a provider will discuss your medication regimen, examine your incision, and assess your muscle and nerve function. You will likely receive a prescription to start physical therapy, a prescription for x-rays and you will schedule your future post-op appointments. X-rays will be ordered at 6 weeks, 3 months, 6 months and 1 year after surgery. Patients with active medical problems should schedule a follow-up appointment with their PCP about 4 weeks after surgery.
If you experience any of the following symptoms:
- Persistent, severe or uncontrollable pain
- Weakness or numbness in your extremities
- Incisional redness, drainage, or increased swelling
- Difficulty breathing, fever, chills
- Problems controlling your bladder or bowel
- No bowel movement for 5 days
- Calf or lower leg swelling
- Take several short walks and perform posture exercises throughout the day.
- Do not lift more than 10 pounds (a gallon of milk weighs about 9 pounds).
- Drink six, 8 oz. glasses of water per day, and eat fresh fruits and vegetables high in fiber.
- Do not participate in sports or activities that require frequent or strenuous bending, twisting, pushing or pulling.
- Limit initial car rides to short, local distances (around 1 hour or less).
- Try to stop wearing your brace, if applicable.
- You may resume intercourse, as tolerated.
- Wean off of all narcotic pain medications and transition to Tylenol/Acetaminophen.
- If you are no longer taking any narcotic pain medication, you may start driving.
- You may go on longer car rides and take short, local flights.
- Do not lift more than 15-20 pounds.
- Start physical therapy.
- You may perform light chores, such as cooking, dusting, sweeping or folding laundry.
- You may participate in non-contact sports and activities such as yoga or cycling.
- If you have a relatively sedentary job, you can likely return to work.
- Gradually increase activities as tolerated by pain.
- You may perform household chores, such as gardening and mowing the lawn, as tolerated by pain.
- You may participate in more non-contact sports and activities such as running, golfing or tennis.
- You may start taking frequent or long distance flights.
- If your job is physically demanding, you can likely return to work.
- You may participate in contact sports, ride a road bicycle, and go downhill skiing, snowmobiling, waterskiing, or horseback riding, as tolerated by pain.
Q:What if I’m not ready to proceed with surgery?
A: You should never feel pressured to proceed with surgery. If you are unsure, we encourage you to review our educational materials, get a second opinion, speak to one or more of our previous surgery patients, or talk with your family and friends./p>
Q: What can I do before my surgery to help with my recovery? (See page titled “Preparing For Surgery”)
A: Dr. Kim recommends maintaining a healthy diet and getting enough sleep each night to strengthen your immune system. You should continue to perform simple stretches and exercises that increase flexibility and strengthen muscles. Keeping your muscles toned and endurance high will help you to recover faster after surgery. Also, you can try to reduce alcohol consumption and try to stop smoking or cut back on the number of cigarettes you smoke each day.
Q: Why should I quit smoking prior to surgery?
A: You should try to stop smoking or cut back on the number of cigarettes you smoke each day, in order to help your bones fuse, wound heal, and minimize the risk of infection. There is a higher chance your fusion will not heal if you continue to smoke because smoking disrupts the normal function of the body’s system, decreases blood flow to healing tissues, limits bone growth and accelerates arthritic changes. Stopping even for a short period of time will be helpful.
Q: Will I see Dr. Kim or a Physician Assistant if I stay overnight in the hospital? (See page titled “Day of Surgery”)
A: Yes! Dr. Kim or one of our Physician Assistants will visit you.
Q: When will I be able to return to my normal activities? (See page titled “After Surgery Do’s and Don’ts”)
A: You can expect to experience less post-operative pain, a shorter hospital stay, a faster recovery time, and an earlier return to work and daily activities than is associated with traditional open back surgery. Nonetheless, it is still surgery. While most procedures successfully relieve pain and improve function, recovery does take time. Returning to your normal activities will be a slow process. Each surgery is different, and the healing and recovery time will vary.
Q: When will I be able to travel? (See page titled “Recovery Guidelines”)
A: You may travel as soon as you feel comfortable, but Dr. Kim recommends avoiding long distance travel for at least 3-4 weeks. During these first few weeks, try to only take short car rides that are 1 hour or less. If you need to take a long care ride, you should stop at least once an hour to stretch and walk around. However, it is okay to fly home after surgery if needed, 24 hours after discharge if you live out of town. Please make sure to get assistance with carrying luggage and consider using a wheelchair support. On the flight, please make sure to walk and stretch every hour.
Q: Will my spinal implant(s) set off metal detectors?
A: Most implants are made of titanium and will not set off metal detectors. If for some reason an alarm does go off, you should inform security of your spinal implant(s) and consider showing them your surgical scar. In some situations, a security guard may wave a wand along your back to confirm your fusion instrumentation.
Q: Why must I take antibiotics for dental work or other surgical procedures?
A: Dental work or other surgeries increases the chance of infection. If an infection spreads to your spinal instrumentation, it must be surgically removed and replaced. Therefore, taking antibiotics reduces the risks of new hardware getting infected. Please inform your dentist and other physicians of your spine surgery. We recommend oral antibiotics prior to invasive dental work for the first year after surgery. Prophylactic antibiotics are not needed after the first year.
