
Back pain can be debilitating, and when conservative treatments fail, spine surgery may become an option. However, before undergoing any spinal procedure, it is critical to accurately identify the source of the pain. This is where diagnostic injections come into play. These injections not only help in pinpointing the exact pain generator but can also offer therapeutic relief. Let’s explore how diagnostic injections are vital when considering spine surgery.
Click here to check out this short video on Why Have Spinal Injections.
The Role of Diagnostic Injections
Diagnostic injections serve two primary purposes:
- Identifying the Pain Generator: These injections can confirm whether the pain originates from a specific area of the spine.
- Providing Therapeutic Relief: Many diagnostic injections contain a combination of an anesthetic to numb the area and a steroid to reduce inflammation, which can relieve pain temporarily.
By offering both diagnostic and therapeutic benefits, these injections help specialists determine the necessity of surgery and the specific area that requires intervention.
Types of Diagnostic Injections Used in Spine Diagnosis
Various diagnostic injections are used depending on the location and type of pain. Here are some commonly used injections in spine care:
- Trigger Point Injection: This injection is used when muscles are the suspected source of pain. The anesthetic and steroid are injected directly into the painful muscle. This injection is performed without imaging and can provide temporary relief to allow the patient to engage in physical therapy.
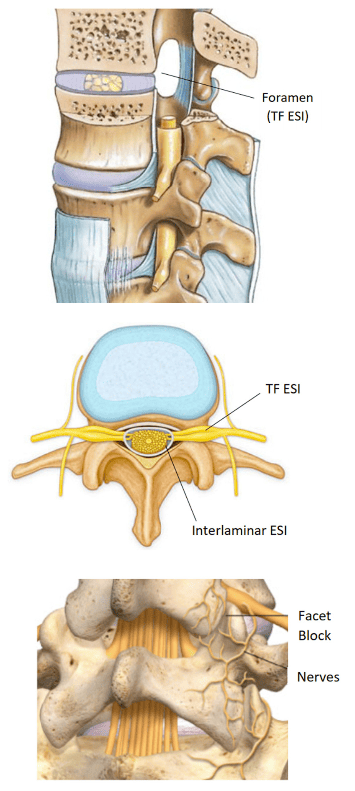
- Epidural Steroid Injection (ESI): ESIs are a widely used option for nerve pain resulting from conditions like herniated discs or spinal stenosis. By reducing inflammation in the affected nerves, ESIs can provide significant relief and help manage pain in the short and long term. This type of injection targets nerve pain caused by inflammation. ESIs come in two types:
- Transforaminal (TF ESI): Injected into the epidural space near the nerve roots.
- Interlaminar ESI: Injected into the interlaminar space, allowing the solution to spread across multiple levels of the spine.
- Facet Injections: These are used to diagnose and treat pain coming from the facet joints (where two vertebrae meet). A facet block injects anesthetic and steroid into the joint, while a Medial Branch Block (MBB) delivers the solution outside the joint, targeting the small nerves transmitting pain signals. These injections not only help confirm that the pain is coming from the facet joint but also provide relief, which allows patients to engage in rehabilitation. For long-term relief, radiofrequency ablation (RFA) can be used to burn the small nerve endings responsible for transmitting pain signals. Although these nerves will regenerate, RFA can offer relief for up to 12 months.
Each of these injections serves a specific role in determining the source of pain and whether surgery is the appropriate solution.
How Diagnostic Injections Work
Diagnostic injections involve two primary components: an anesthetic to numb the pain and a steroid to reduce inflammation. The injection is usually administered at the suspected pain site, and the patient is monitored for their response to the anesthetic during the first few hours after the injection.
- Diagnostic Information: The first few hours after the injection are crucial. If the patient experiences significant pain relief during this time, it indicates that the injected area is likely the pain generator.
- Therapeutic Benefit: Beyond diagnostics, the steroid may provide longer-term pain relief by reducing inflammation, often allowing the patient to participate more effectively in physical therapy.
If the pain persists after the injection, it signals that the pain source may lie elsewhere, leading the physician to re-evaluate the condition.
Diagnostic Accuracy and Pain Localization
The main objective of diagnostic injections is to accurately localize the source of pain. If the patient reports that they are pain-free during the anesthetic’s numbing effect (usually lasting 2–4 hours), the injection has successfully identified the pain generator. However, if no improvement is seen, the specialist will investigate other potential causes.
Therapeutic Benefits of Injections
While the primary function of these injections is diagnostic, the therapeutic benefit is significant. The steroid component in the injection can begin to work a few days after the procedure, offering long-term pain relief by decreasing inflammation. This window of pain relief can be crucial for patients to participate in physical therapy, strengthening their core muscles to provide natural support to the spine.
Benefits of Diagnostic Injections Before Spine Surgery
Diagnostic injections are a crucial step before committing to spine surgery. They help confirm the exact location of the pain, ensuring that surgery is necessary and precisely targeted. By offering a non-invasive diagnostic tool, these injections minimize the risk of unnecessary surgeries, improving the overall success rate of spinal interventions.
Risks and Considerations
As with any medical procedure, diagnostic injections carry some risks. Side effects may include infection, bleeding, or a temporary increase in pain. Patients on blood thinners or NSAIDs may need to stop their medications prior to the injection. It’s essential to discuss any potential risks with your doctor before proceeding with the injection.
When to Consider Spine Surgery After Injections
Diagnostic injections play a pivotal role in deciding whether surgery is the best course of action. If the injection successfully alleviates pain, it not only confirms the source but also informs the surgeon about the area that may need surgical intervention. In cases where pain relief is temporary or partial, injections can still provide valuable information about the condition and inform the next steps.
Physical Therapy Post-Injection
After receiving pain relief from an injection, patients are often encouraged to engage in a physical therapy program. Strengthening the core muscles is vital for maintaining spine health and preventing future issues. Physical therapy, combined with the therapeutic effects of the injection, can significantly improve long-term outcomes.
The Importance of a Multidisciplinary Approach
Managing spine conditions effectively often requires a multidisciplinary approach that includes diagnostic injections, physical therapy, and possibly surgery. Pain specialists, physical therapists, and surgeons work together to ensure the best outcome for the patient, with diagnostic injections serving as a critical step in this collaborative process.
Conclusion
Diagnostic injections are an essential tool when considering spine surgery. Not only do they help pinpoint the exact source of pain, but they also provide therapeutic benefits that can reduce inflammation and allow patients to engage in effective physical therapy. By helping to clarify the need for surgery, these injections improve outcomes and ensure that the chosen treatment plan is both targeted and effective. If you’re considering spine surgery, diagnostic injections may be the key to determining whether surgery is necessary and, if so, how best to approach it.
FAQs
What are diagnostic injections, and how do they work? Diagnostic injections are medical procedures used to pinpoint the source of spinal pain. They involve injecting a combination of anesthetic (to numb the area) and a steroid (to reduce inflammation). If the pain subsides after the injection, it confirms that the targeted area is the pain generator, helping doctors determine the best treatment, including surgery.
Why are diagnostic injections important before spine surgery? Diagnostic injections are crucial because they help accurately identify the source of pain. By confirming the exact location of the issue, they allow doctors to avoid unnecessary surgeries and ensure that any surgical procedure is targeted and precise, leading to better outcomes.
How soon will I feel relief after a diagnostic injection? You may feel relief from the anesthetic within 15-30 minutes after the injection, which lasts a few hours. The steroid component takes longer to work, typically providing relief within 2-5 days after the procedure, and its effects can last for weeks or months depending on the individual and the condition being treated.
How long does the relief from a diagnostic injection last? The pain relief from a diagnostic injection can vary. The anesthetic provides temporary relief lasting a few hours, while the steroid can offer longer-term relief, typically starting a few days after the injection and lasting several weeks or months. However, the primary purpose is to diagnose the pain generator rather than provide long-term pain management.
Are there any risks or side effects associated with diagnostic injections? As with any medical procedure, diagnostic injections carry some risks, including infection, bleeding, or temporary increased pain. Patients on blood thinners or NSAIDs need to stop their medications before the injection. It’s essential to discuss any potential risks with your doctor before undergoing the procedure.
What happens after I receive a diagnostic injection? After the injection, your doctor will ask you to monitor your pain levels closely over the next few hours and days. If the pain subsides immediately after the injection, it confirms the source of your pain. Depending on the results, you may be advised to undergo physical therapy or, in some cases, discuss surgical options.
Will I need surgery if my diagnostic injection provides relief? Not necessarily. If the diagnostic injection provides significant pain relief, it may indicate that non-surgical treatments, such as physical therapy, could be effective. However, if relief is temporary or partial, surgery may still be recommended to address the underlying issue more permanently.
Are diagnostic injections painful? The procedure may involve some discomfort, but most patients find the pain to be minimal and tolerable. A local anesthetic is used to numb the injection site, and any discomfort during the procedure is generally brief. Some soreness at the injection site is common after the procedure, but it typically subsides within a day or two.
What should I do if the diagnostic injection doesn’t relieve my pain? If the injection does not provide pain relief, it indicates that the targeted area may not be the source of your pain. Your doctor will reassess the situation and may recommend further diagnostic tests or injections in different areas to accurately locate the pain generator.
How do I prepare for a diagnostic injection? Before your diagnostic injection, your doctor will likely ask you to stop taking certain medications, such as blood thinners or NSAIDs, to reduce the risk of bleeding. You should also inform your healthcare provider about any allergies or medical conditions. On the day of the injection, it’s best to have someone accompany you to drive you home after the procedure.
What is the difference between a diagnostic and a therapeutic injection? A diagnostic injection is performed to identify the exact location of the pain, using a local anesthetic to temporarily numb the area. A therapeutic injection aims to provide longer-lasting pain relief and typically contains a steroid to reduce inflammation. Many injections, however, serve both diagnostic and therapeutic purposes.
How many diagnostic injections will I need? In most cases, one or two diagnostic injections are enough to identify the pain source. However, if the first injection does not provide conclusive results, additional injections may be necessary to further investigate the pain generator.
Who is a good candidate for diagnostic injections? Patients with chronic back or neck pain that has not responded to conservative treatments (such as physical therapy, medication, or rest) are typically good candidates for diagnostic injections. These injections are especially helpful in determining the need for spine surgery.
