What Is Spinal Stenosis?
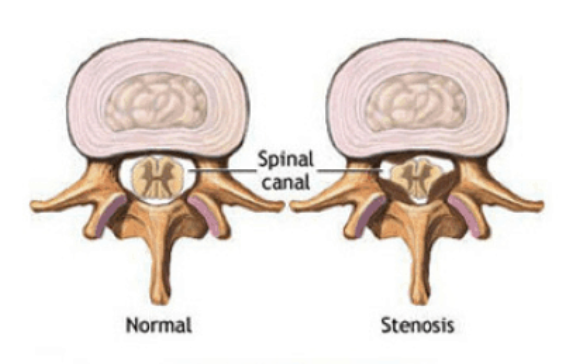
Spinal stenosis is a condition where the space within the spinal canal becomes narrowed, which can put pressure on the spinal cord or nearby nerves. This compression may lead to symptoms such as pain, numbness, tingling, or weakness in the neck, back, arms, or legs. Stenosis most commonly affects the cervical spine (neck) and lumbar spine (lower back).
What Causes Spinal Stenosis?
Spinal stenosis is usually caused by age-related changes in the spine, but it can also result from structural problems or previous injuries. Common causes include:
- Degenerative disc bulging
- Herniated discs
- Facet joint arthritis (facet arthropathy)
- Thickened ligaments
- Vertebral misalignment such as spondylolisthesis
These changes can reduce the amount of space available for the spinal cord and nerves, causing irritation and compression that leads to symptoms.
What Are the Signs and Symptoms of Spinal Stenosis?
Symptoms of spinal stenosis can vary depending on where the narrowing occurs and how severe it is. Some people may not experience symptoms at all, especially if the narrowing develops slowly and the body adapts. Others may experience:
- Pain, numbness, tingling, or weakness in the arms or legs
- Radiating nerve pain (radiculopathy)
- Heaviness or fatigue in the legs when walking (neurogenic claudication)
- Gait instability, poor coordination, or difficulty with fine motor tasks like handwriting or buttoning clothes (myelopathy)
Cervical stenosis typically affects the neck, shoulders, arms, and hands, while lumbar stenosis tends to affect the lower back, buttocks, and legs.
What Are the Risk Factors for Spinal Stenosis?
Several factors may increase the likelihood of developing spinal stenosis, including:
- Natural aging and disc degeneration
- Arthritis of the spine
- Previous spinal injuries or surgeries
- Congenital narrowing of the spinal canal
- Scoliosis or other spinal deformities
- Repetitive strain or poor posture over time
How Is Spinal Stenosis Diagnosed?
Diagnosis starts with a thorough medical history and physical exam to assess symptoms, posture, nerve function, strength, and flexibility. Imaging studies are often used to confirm the diagnosis and identify the specific location of the narrowing. These may include:
- X-rays to check alignment and joint degeneration
- MRI scans to evaluate soft tissues and nerve compression
- CT scans to provide detailed images of bone structures
This information helps guide treatment and determine the best course of action.
What Are the Treatment Options for Spinal Stenosis?
Many people with spinal stenosis improve with non-surgical treatments. Treatment plans are tailored to each patient’s symptoms, lifestyle, and goals.
Non-Surgical Treatments May Include:
- Physical therapy to strengthen core muscles and support the spine
- Anti-inflammatory medications to reduce swelling and discomfort
- Epidural steroid injections to calm irritated nerves
- Activity modification and ergonomic changes to reduce stress on the spine
Surgical Treatment:
Surgery may be recommended if symptoms do not improve with conservative treatment, or if there is progressive weakness, numbness, or loss of bowel or bladder control.
In the lumbar spine, a decompression procedure called a laminectomy is often used to relieve pressure on the nerves. If instability is present, a spinal fusion may also be necessary.
In the cervical spine, because of the delicate nature of the spinal cord, surgery is typically performed from the front of the neck using techniques like anterior cervical discectomy and fusion (ACDF) or cervical disc replacement.

What Is the Recovery Process After Surgery for Stenosis?
Recovery varies depending on the surgical approach and the patient’s overall health. Most patients are encouraged to begin walking shortly after surgery. Physical therapy is often part of the recovery process and helps improve mobility, strengthen muscles, and support spinal alignment.
Patients typically return to light activities within a few weeks and gradually resume more strenuous activity under the guidance of their spine specialist.
Are There Ways to Help Prevent Spinal Stenosis?
While not all cases can be prevented, there are steps that may help reduce the risk or slow the progression of spinal stenosis:
- Maintain good posture and spinal alignment
- Exercise regularly to keep muscles strong and flexible
- Strengthen the core and back muscles
- Avoid smoking, which accelerates spinal degeneration
- Maintain a healthy weight to reduce stress on the spine
Making these healthy lifestyle choices can support long-term spinal health and reduce the risk of developing or worsening spinal stenosis.
What Happens If Spinal Stenosis Is Left Untreated?
If spinal stenosis is left untreated, symptoms may gradually worsen. Persistent compression of the spinal cord or nerves can lead to:
- Chronic pain and discomfort
- Reduced mobility and independence
- Nerve damage resulting in permanent numbness or weakness
- Difficulty walking or performing daily tasks
- In severe cases, loss of bladder or bowel control
Early diagnosis and treatment can help prevent complications and improve quality of life.
Are There Conditions Related to Spinal Stenosis?
Spinal stenosis is often associated with or occurs alongside other spinal conditions, such as:
- Herniated discs
- Spondylolisthesis (slipped vertebra)
- Degenerative disc disease
- Facet joint syndrome
- Myelopathy or radiculopathy
Comprehensive evaluation ensures that all contributing factors are identified and treated appropriately.
Key Takeaways About Spinal Stenosis
- Spinal stenosis is a narrowing of the spinal canal that can compress the spinal cord or nerves.
- It is commonly caused by disc bulges, arthritis, and misalignment in the spine.
- Symptoms include pain, numbness, leg heaviness, or coordination problems, depending on the location of the stenosis.
- Non-surgical treatments are effective for many patients, and surgery is available when necessary.
- Preventative care and early intervention can help maintain spinal health and avoid long-term complications.
Next Steps
If you are experiencing ongoing back or neck pain, leg weakness, or difficulty walking, schedule a consultation with a spine specialist to explore your treatment options. Early evaluation and a personalized care plan can help you feel better, move better, and get back to doing what you love.

